The term angina pectoris or angina is used to describe chest pain or discomfort, often felt like a pressure or a squeezing sensation in the chest. The pain may radiate to the shoulders, arms, neck, jaw or the back region between the shoulder blades.
Typically, a patient with angina will experience no symptoms at rest. However, during exercise, the oxygen demands of the heart muscle will increase.

If blood supply in a coronary artery is limited, usually because of an atherosclerotic plaque, angina will occur.
Causes of chest pain can be related to a variety of symptoms. Over six million people visit hospital emergency annually because of chest pain.
Causes of chest pain can vary from life-threatening conditions to those that are relatively harmless. The most common causes of chest pain are musculoskeletal (30-50%) and gastrointestinal conditions (10-20%).
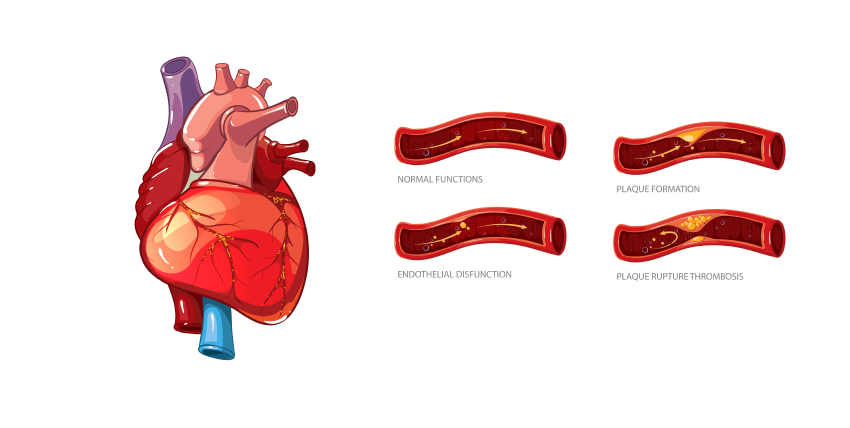
Cholesterol-containing deposits (plaque) in your arteries and inflammation are usually to blame for coronary artery disease.
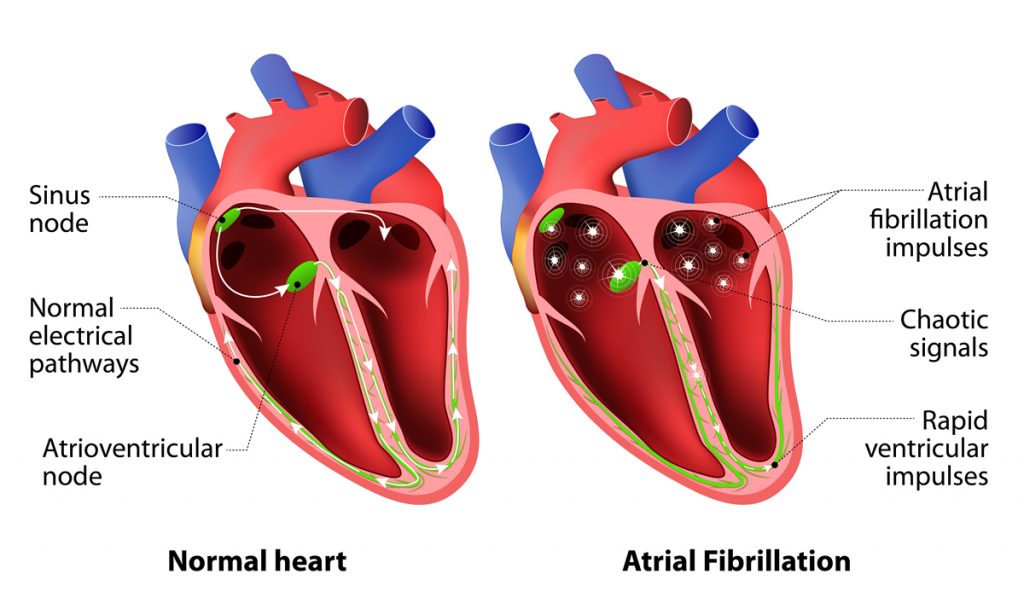
Atrial fibrillation, or Afib, is an irregular, rapid heart rate. This can be caused by an overactive thyroid gland or other metabolic imbalance. Exposure to stimulants, such as medications, caffeine, tobacco or alcohol.In excess of two million Americans are suffering from AFib. More common in the elderly, 60 and older. AFib is Atrial fibrillation, and it is a quivery, fluttery heartbeat.
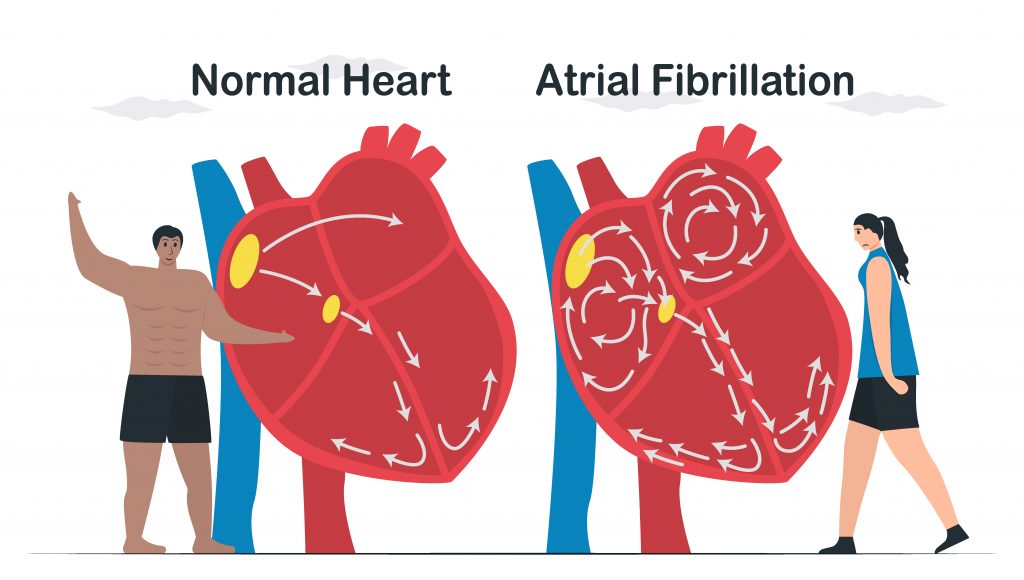
You may hear the doctor call it arrhythmia. It means your heart’s rhythm is abnormal, and your blood isn’t moving well. What exactly happens with AFib? The top part of your heart, the atria, squeezes first, and then the bottom part the ventricles. The timing of these contractions is what moves the blood. With AFib, the signals that control this process are off schedule. Instead of working together, they do their own thing. Symptoms of Afib can cause heart failure.
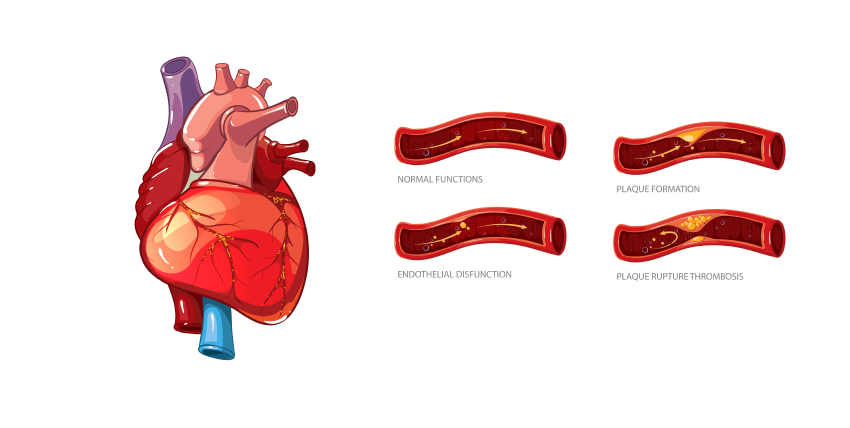
Coronary artery disease develops when the major blood vessels that supply your heart with blood, oxygen, and nutrients (coronary arteries) become damaged or diseased.When plaque builds up, it narrows your coronary arteries, decreasing blood flow to your heart. Eventually, the reduced blood flow may cause chest pain (angina), shortness of breath, or other coronary artery disease signs and symptoms.
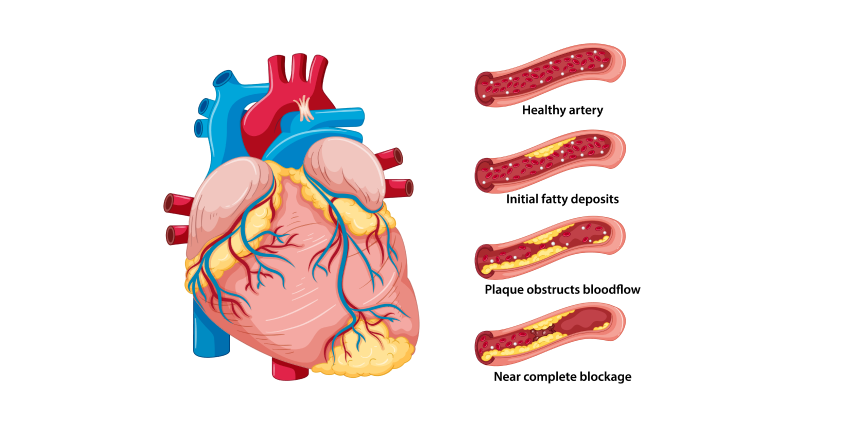
A complete blockage can cause a heart attack.Cholesterol-containing deposits (plaque) in your arteries and inflammation are usually to blame for coronary artery disease.Because coronary artery disease often develops over decades, you might not notice a problem until you have a significant blockage or a heart attack. However, there’s plenty you can do to prevent and treat coronary artery disease. A healthy lifestyle can make a substantial impact.
Cholesterol is a waxy substance found in your blood. Your body needs cholesterol to build healthy cells, but high levels of cholesterol can increase your risk of heart disease.With high cholesterol, you can develop fatty deposits in your blood vessels. Eventually, these deposits grow, making it difficult for enough blood to flow through your arteries.
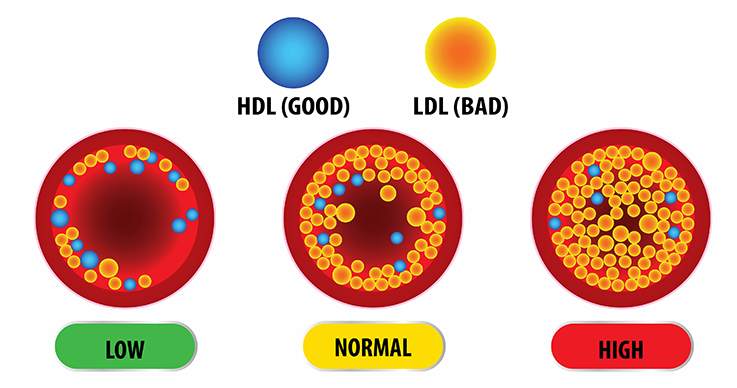
Sometimes, those deposits can break suddenly and form a clot that causes a heart attack or stroke.High cholesterol can be inherited, but it’s often the result of unhealthy lifestyle choices, which make it preventable and treatable. A healthy diet, regular exercise and sometimes medication can help reduce high cholesterol.
Causes of chest pain can vary from life-threatening conditions to those that are relatively harmless. The most common causes of chest pain are musculoskeletal (30-50%) and gastrointestinal conditions (10-20%).
When plaque builds up, it narrows your coronary arteries, decreasing blood flow to your heart. Eventually, the reduced blood flow may cause chest pain (angina), shortness of breath, or other coronary artery disease signs and symptoms. A complete blockage can cause a heart attack.

Heart failure, sometimes known as congestive heart failure, happens when your heart muscle doesn’t pump blood efficiently as it should. Certain conditions, such as narrowed arteries in your heart (coronary artery disease) or high blood pressure, gradually leave your heart too weak or stiff to fill and pump efficiently.

Not all conditions that lead to heart failure can be reversed, but treatments can improve the signs and symptoms of heart failure and help you live longer. Lifestyle changes — such as exercising, reducing sodium in your diet, managing stress and losing weight — can improve your quality of life.
One way to prevent heart failure is to prevent and control conditions that cause heart failures, such as coronary artery disease, high blood pressure, diabetes or obesity.
Although these signs and symptoms may be due to heart failure, there are many other possible causes, including other life-threatening heart and lung conditions. Don’t try to diagnose yourself. Call 911 or your local emergency number for immediate help. Emergency room doctors will try to stabilize your condition and determine if your symptoms are due to heart failure or something else.
A stroke occurs when the blood supply to part of your brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. Brain cells begin to die in minutes.A stroke is a medical emergency, and prompt treatment is crucial. Early action can reduce brain damage and other complications.The good news is that many fewer Americans die of stroke now than in the past.

Peripheral artery disease (also called peripheral arterial disease) is a common circulatory problem in which narrowed arteries reduce blood flow to your limbs.When you develop peripheral artery disease (PAD), your legs or arms — usually your legs — don’t receive enough blood flow to keep up with demand. This may cause symptoms, such as leg pain when walking (claudication).

Peripheral artery disease is also likely to be a sign of a buildup of fatty deposits in your arteries (atherosclerosis). This condition may narrow your arteries and reduce blood flow to your legs and, occasionally, your arms.


The condition is very common, especially in women. Around 25 percent of all adults have varicose veins. In most cases, varicose veins appear on the lower legs.
Varicose veins occur when veins aren’t functioning properly. Veins have one-way valves that prevent blood from flowing backward. When these valves fail, blood begins to collect in the veins rather than continuing toward your heart. The veins then enlarge. Varicose veins often affect the legs. The veins there are the farthest from your heart, and gravity makes it harder for the blood to flow upward.
The primary symptoms of varicose veins are highly visible, misshapen veins, usually on your legs. You may also have pain, swelling, heaviness, and achiness over or around the enlarged veins.In some cases, you can develop swelling and discoloration. In severe cases, the veins can bleed significantly, and ulcers can form.
Venous insufficiency is the inadequate circulation of venous blood back to the heart. Venous insufficiency occurs most often in the legs and, less commonly, in other parts of the body. Venous insufficiency can be caused by factors that impair venous return (the return of blood to the heart) or factors that increase blood volume/pressure (peripheral edema).

Venous insufficiency is also called chronic venous disease, chronic refers to damage that has been present for several months.Venous insufficiency can cause cosmetic problems including leg swelling and skin changes, but it may also lead to serious medical conditions including skin ulcers or cellulitis. Venous insufficiency can be difficult to diagnose because symptoms are often nonspecific.Venous insufficiency is frequently “silent,” that is, it is asymptomatic.
Symptoms of Venous Insufficiency The following are the most common symptoms of Venous Insufficiency – Pain – Swelling – Skin changes including discoloration, redness, thinning skin, and varicose veins or thickened veins under the skin’s surface (striae) – Itchy skin (pruritus) – Dry scaly skin (xerosis) – Blood clots in the legs (deep vein thrombosis [DVT]) – Chronic leg ulcers – Warm skin around the ankle, where a vein has been removed (phlebitis) – Venous stasis dermatitis, which presents with itchy or scaly red patches on the lower leg that may ooze fluid and become crusty if scratched – Venous insufficiency can be divided into three types: superficial reflux, deep venous insufficiency, cavernous incompetence.
Symptoms are determined by which type of cause of Venous Insufficiency is present. Some patients have no symptoms at all. This is called “claudication.” When they do occur, symptoms usually develop slowly over years. Symptoms may include pain in the legs, swelling, burning sensations in the legs, skin changes, discoloration of the skin on the lower leg or foot, redness or scaling of the skin on the lower leg or foot.
Atrial fibrillation, or Afib, is an irregular, rapid heart rate. This can be caused by an overactive thyroid gland or other metabolic imbalance. Exposure to stimulants, such as medications, caffeine, tobacco or alcohol.In excess of two million Americans are suffering from AFib. More common in the elderly, 60 and older. AFib is Atrial fibrillation, and it is a quivery, fluttery heartbeat.
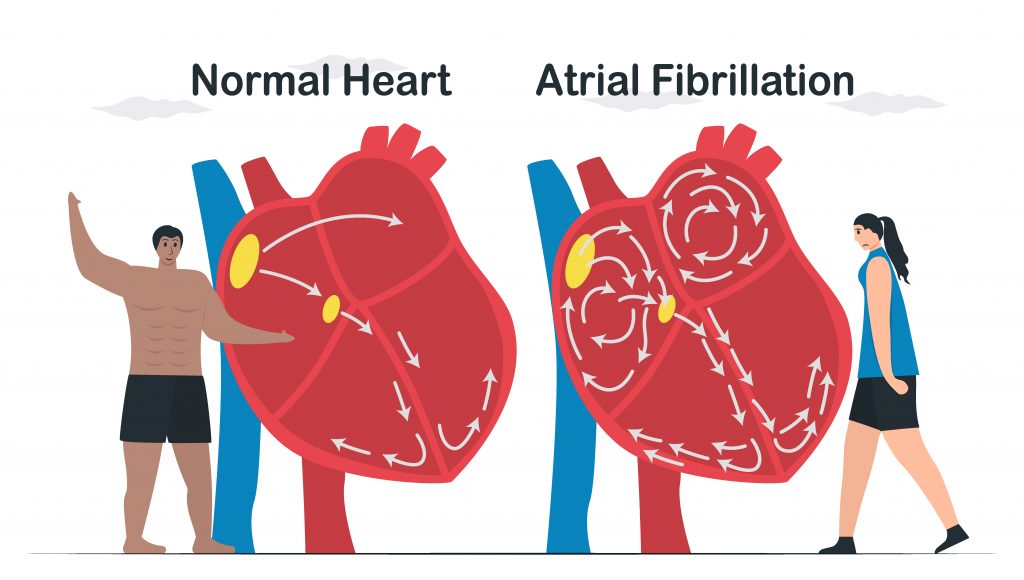
You may hear the doctor call it arrhythmia. It means your heart’s rhythm is abnormal, and your blood isn’t moving well. What exactly happens with AFib? The top part of your heart, the atria, squeezes first, and then the bottom part the ventricles. The timing of these contractions is what moves the blood. With AFib, the signals that control this process are off schedule. Instead of working together, they do their own thing. Symptoms of Afib can cause heart failure.
Atrial fibrillation, or Afib, is an irregular, rapid heart rate. This can be caused by an overactive thyroid gland or other metabolic imbalance. Exposure to stimulants, such as medications, caffeine, tobacco or alcohol.In excess of two million Americans are suffering from AFib. More common in the elderly, 60 and older. AFib is Atrial fibrillation, and it is a quivery, fluttery heartbeat.
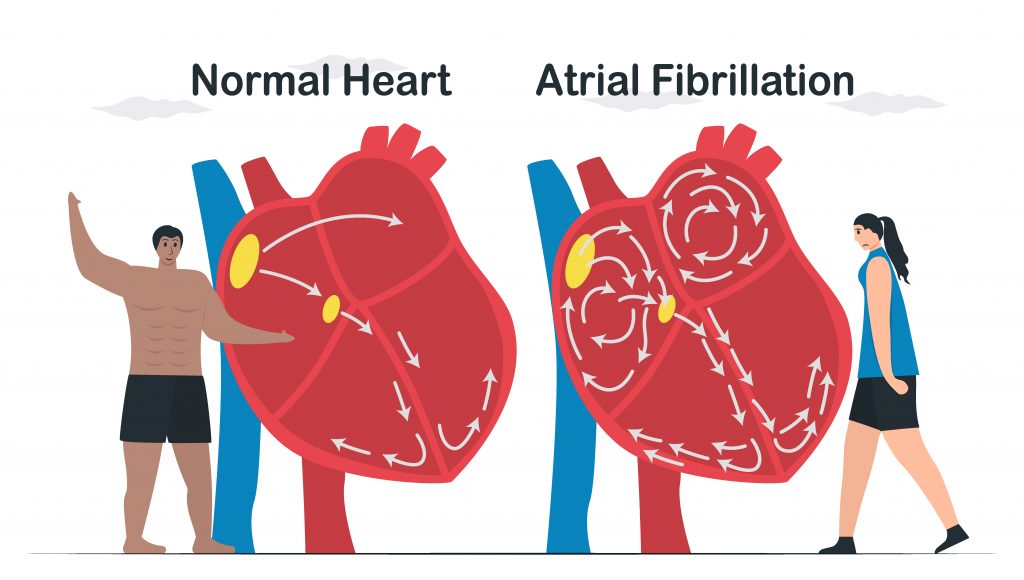
You may hear the doctor call it arrhythmia. It means your heart’s rhythm is abnormal, and your blood isn’t moving well. What exactly happens with AFib? The top part of your heart, the atria, squeezes first, and then the bottom part the ventricles. The timing of these contractions is what moves the blood. With AFib, the signals that control this process are off schedule. Instead of working together, they do their own thing. Symptoms of Afib can cause heart failure.
Cholesterol is a waxy substance found in your blood. Your body needs cholesterol to build healthy cells, but high levels of cholesterol can increase your risk of heart disease.With high cholesterol, you can develop fatty deposits in your blood vessels. Eventually, these deposits grow, making it difficult for enough blood to flow through your arteries.
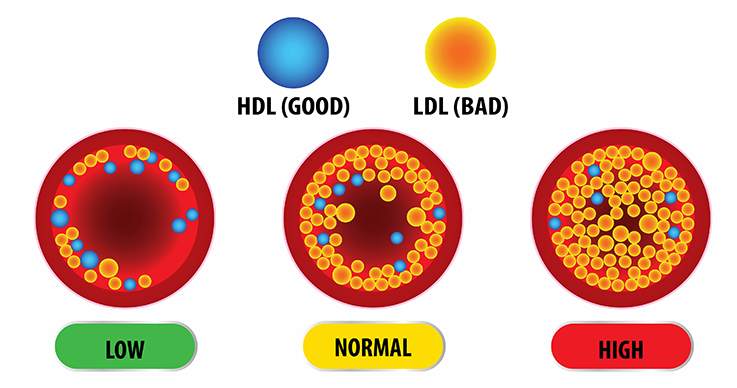
Sometimes, those deposits can break suddenly and form a clot that causes a heart attack or stroke.High cholesterol can be inherited, but it’s often the result of unhealthy lifestyle choices, which make it preventable and treatable. A healthy diet, regular exercise and sometimes medication can help reduce high cholesterol.
Causes of chest pain can vary from life-threatening conditions to those that are relatively harmless. The most common causes of chest pain are musculoskeletal (30-50%) and gastrointestinal conditions (10-20%).
When plaque builds up, it narrows your coronary arteries, decreasing blood flow to your heart. Eventually, the reduced blood flow may cause chest pain (angina), shortness of breath, or other coronary artery disease signs and symptoms. A complete blockage can cause a heart attack.

Heart failure, sometimes known as congestive heart failure, happens when your heart muscle doesn’t pump blood efficiently as it should. Certain conditions, such as narrowed arteries in your heart (coronary artery disease) or high blood pressure, gradually leave your heart too weak or stiff to fill and pump efficiently.

Not all conditions that lead to heart failure can be reversed, but treatments can improve the signs and symptoms of heart failure and help you live longer. Lifestyle changes — such as exercising, reducing sodium in your diet, managing stress and losing weight — can improve your quality of life.
One way to prevent heart failure is to prevent and control conditions that cause heart failures, such as coronary artery disease, high blood pressure, diabetes or obesity.
Although these signs and symptoms may be due to heart failure, there are many other possible causes, including other life-threatening heart and lung conditions. Don’t try to diagnose yourself. Call 911 or your local emergency number for immediate help. Emergency room doctors will try to stabilize your condition and determine if your symptoms are due to heart failure or something else.
Peripheral artery disease (also called peripheral arterial disease) is a common circulatory problem in which narrowed arteries reduce blood flow to your limbs.When you develop peripheral artery disease (PAD), your legs or arms — usually your legs — don’t receive enough blood flow to keep up with demand. This may cause symptoms, such as leg pain when walking (claudication).

Peripheral artery disease is also likely to be a sign of a buildup of fatty deposits in your arteries (atherosclerosis). This condition may narrow your arteries and reduce blood flow to your legs and, occasionally, your arms.
A stroke occurs when the blood supply to part of your brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. Brain cells begin to die in minutes.A stroke is a medical emergency, and prompt treatment is crucial. Early action can reduce brain damage and other complications.The good news is that many fewer Americans die of stroke now than in the past.



The condition is very common, especially in women. Around 25 percent of all adults have varicose veins. In most cases, varicose veins appear on the lower legs.
Varicose veins occur when veins aren’t functioning properly. Veins have one-way valves that prevent blood from flowing backward. When these valves fail, blood begins to collect in the veins rather than continuing toward your heart. The veins then enlarge. Varicose veins often affect the legs. The veins there are the farthest from your heart, and gravity makes it harder for the blood to flow upward.
The primary symptoms of varicose veins are highly visible, misshapen veins, usually on your legs. You may also have pain, swelling, heaviness, and achiness over or around the enlarged veins.In some cases, you can develop swelling and discoloration. In severe cases, the veins can bleed significantly, and ulcers can form.
Venous insufficiency is the inadequate circulation of venous blood back to the heart. Venous insufficiency occurs most often in the legs and, less commonly, in other parts of the body. Venous insufficiency can be caused by factors that impair venous return (the return of blood to the heart) or factors that increase blood volume/pressure (peripheral edema).

Venous insufficiency is also called chronic venous disease, chronic refers to damage that has been present for several months.Venous insufficiency can cause cosmetic problems including leg swelling and skin changes, but it may also lead to serious medical conditions including skin ulcers or cellulitis. Venous insufficiency can be difficult to diagnose because symptoms are often nonspecific.Venous insufficiency is frequently “silent,” that is, it is asymptomatic.
Symptoms of Venous Insufficiency The following are the most common symptoms of Venous Insufficiency – Pain – Swelling – Skin changes including discoloration, redness, thinning skin, and varicose veins or thickened veins under the skin’s surface (striae) – Itchy skin (pruritus) – Dry scaly skin (xerosis) – Blood clots in the legs (deep vein thrombosis [DVT]) – Chronic leg ulcers – Warm skin around the ankle, where a vein has been removed (phlebitis) – Venous stasis dermatitis, which presents with itchy or scaly red patches on the lower leg that may ooze fluid and become crusty if scratched – Venous insufficiency can be divided into three types: superficial reflux, deep venous insufficiency, cavernous incompetence.
Symptoms are determined by which type of cause of Venous Insufficiency is present. Some patients have no symptoms at all. This is called “claudication.” When they do occur, symptoms usually develop slowly over years. Symptoms may include pain in the legs, swelling, burning sensations in the legs, skin changes, discoloration of the skin on the lower leg or foot, redness or scaling of the skin on the lower leg or foot.