An Adenosine Myocardial Perfusion Imaging test uses a radioactive imaging agent (not a dye) to produce pictures of the heart muscle. The imaging agent gives off a small amount of radiation which can be seen with a special camera. The amount of radiation exposure during this test is very small and poses no health risk.

The test will help your doctor determine if there are areas of your heart that do not receive enough blood supply due to coronary artery disease. Areas of your heart that may have been damaged from a previous heart attack may also be seen.
Prior to the test, an IV will be started. During the rest portion of the test, you will receive an injection of the radioactive imaging agent, and pictures will be taken of your heart. For the stress portion of the test, a medication (Adenosine) will be given through the IV to simulate exercise by dilating the blood vessels of the heart. During the infusion, you will be continuously monitored for blood pressure, heart rate, rhythm, and ECG changes.

Carotid ultrasonography (carotid U/S) is an ultrasound of the carotid arteries. Carotids are the arteries in your neck that supply blood to your brain. A small transducer, similar to the one used for listening with a stethoscope, is placed on the patient’s neck next to their windpipe (trachea).

A Cardiac Catheterization allows a physician to examine a patient’s heart for pumping function, check for blockage in the arteries bringing blood to the heart, and measure pressures within the heart. Patients are usually given a mild sedative prior to the procedure. This will help you feel more relaxed and maybe a bit sleepy.This test is done in a room with special cameras to take x-ray pictures of your heart.
The nurse or technician will cleanse and shave the area and cover you with sterile drapes. The doctor will then numb the area and insert a small hollow tube or sheath into the artery in your groin (or arm). The physician can then thread special catheters (long, thin plastic tubes) up to the heart.This test is done in a room with special cameras to take x-ray pictures of your heart. Most cardiac catheterizations are done through a large artery in the groin, However Dr. De is known for being one of the few who prefer the radial approach, done through the wrist.
Through these specially shaped catheters, the physician can inject x-ray contrast dye and take x-ray pictures of the arteries that supply blood to the heart muscle and the main pumping chamber of the heart. Some people may notice a mild discomfort or “hot flash” following the dye injection which will last only a few seconds.
During the catheterization, the physician can view the x-ray images on special TV screens. The entire procedure can take as little as 20 minutes or sometimes more than an hour, depending on how many and what type of measurements are taken. After the physician has completed the procedure, the sheaths are removed from the groin (or arm) and a nurse or cath lab technician will hold pressure on the site to allow the small hole in the artery to close. A special dressing, pressure device or sandbag may be placed on the site at this time.
You will be asked to lie flat and still for several hours after the procedure to allow the hole in the artery to seal. Some physicians use a type of vascular closure device to seal the puncture in the artery. You should follow your physician’s specific instructions about activity following the use of one of these devices.
Most patients will go home several hours after the procedure, but because you have been given medication to relax you, please plan to have someone drive you home.

People who have had unexplained fainting spells or heart palpitations that can’t be detected by short term heart rhythm recording devices—such as Holter monitors—may be candidates for this device. Doctors may also recommend an implantable loop recorder for people with atrial fibrillation, which causes a rapid and irregular heartbeat. In addition, this device is used in people who have had a stroke for which a cause has not been determined.
Your doctor makes a small incision in the upper chest and inserts the device just under the skin. This is a brief, outpatient procedure done in our office, you can return to your usual activities the next day. Your doctor may limit your activity until the incision heals.
Cardiac loop recorders typically monitor the heart’s electrical activity for up to 36 months before replacement is required. The device is removed through the original incision site through a short surgery that is similar to the implantation procedure.

What is Peripheral Vascular Intervention?
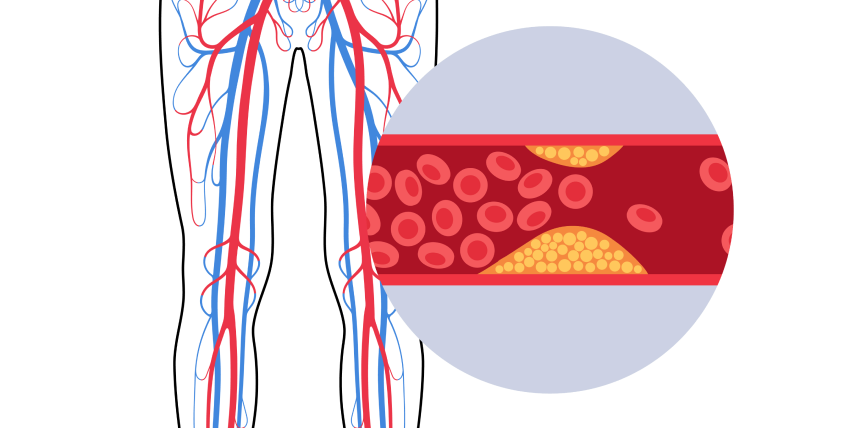
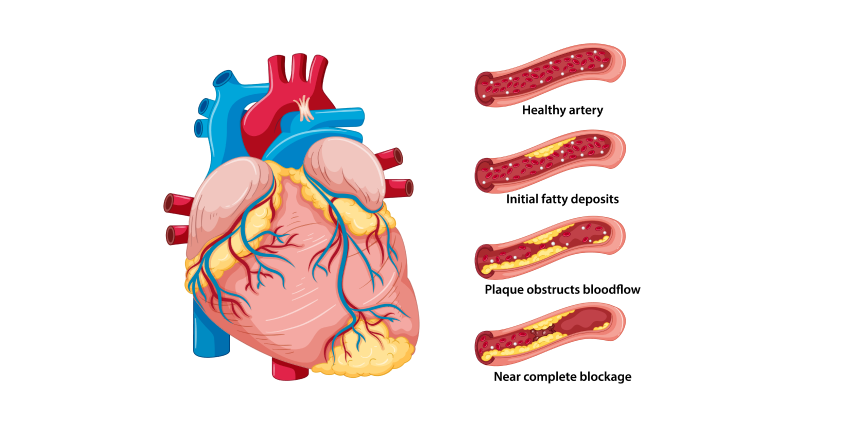
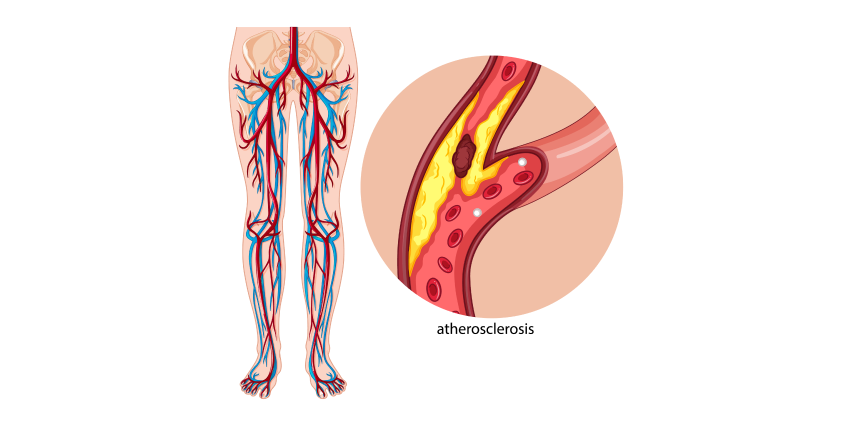
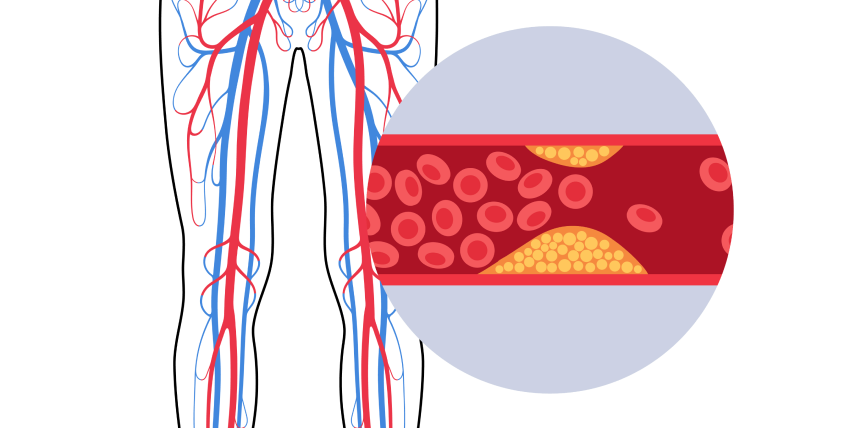
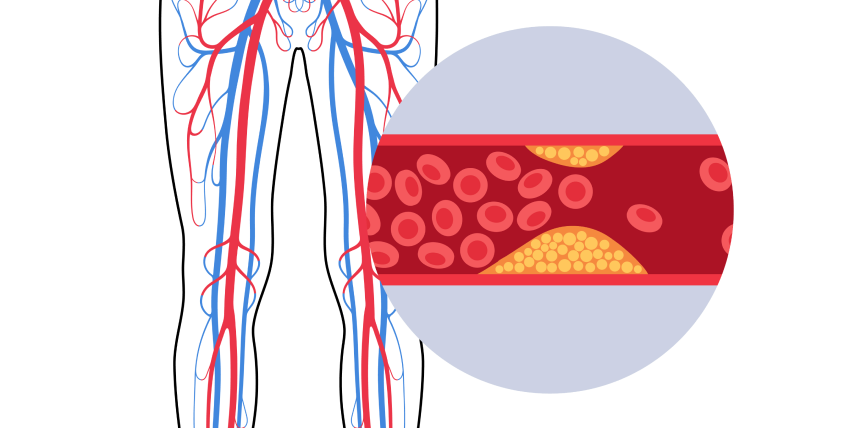
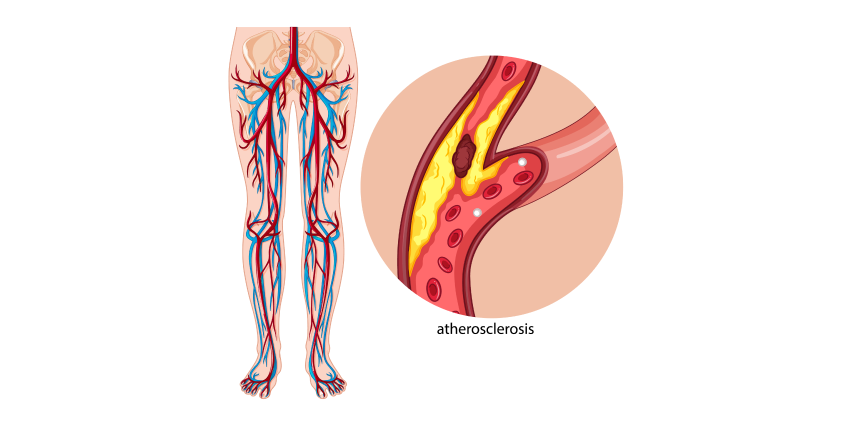
Peripheral vascular intervention is a minimally invasive outpatient (same day) procedure used to treat peripheral artery disease, which causes plaque buildup in the arteries leading to the intestines, head, arms, and most commonly the legs. Plaque buildup is also called atherosclerosis.
The goal of peripheral vascular intervention is to restore the flow of blood to your lower extremities, eliminating pain, numbness, or need for amputation. Our specialists typically employ two different methods – angioplasty and atherectomy.
Angioplasty & Stents
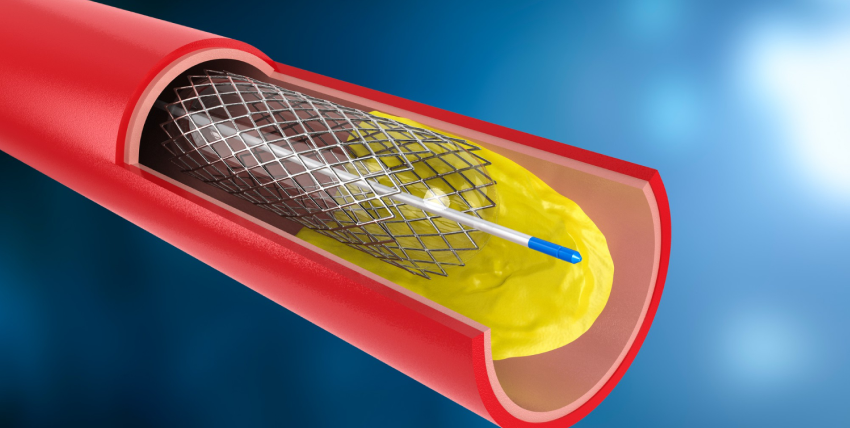
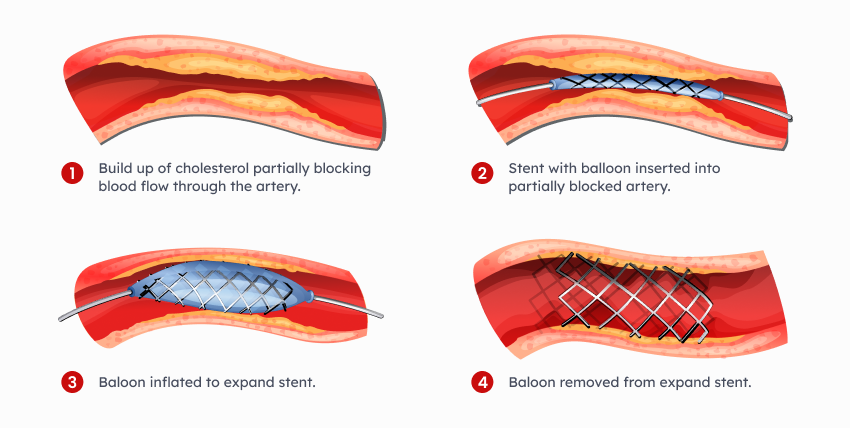
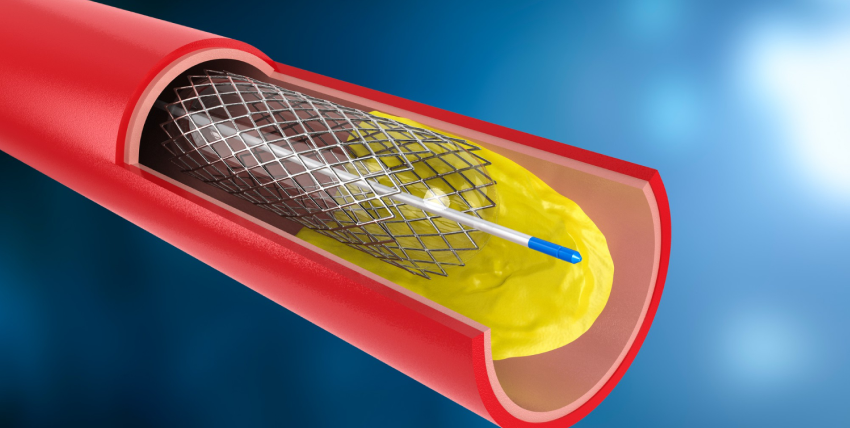
Angioplasty is a minimally invasive intervention method that uses a balloon-tipped catheter to dilate your artery. Once inserted, the balloon is inflated at the blockage site to compress the plaque against the wall of the artery, increasing the flow of blood. In order to prevent the artery from becoming blocked again long-term, a small tube called a stent is sometimes put in place.
Atherectomy
Atherectomy is a non-surgical intervention that removes plaque using a catheter with either a sharp blade or a small drill on its tip. The plaque is either captured by the end of a catheter or is broken up and safely released into the bloodstream.


The sound waves reflect (echo) off the tissues and organs to create pictures which can be seen on a screen. The TEE provides very clear pictures of the heart structures and blood flow. The pictures are usually clearer than those obtained from a standard echocardiogram, which is performed from the chest wall. This test is often used to view hard-to-see structures or to obtain more detailed pictures of the heart and aorta.
Common reasons for the test include measuring the size and pumping strength of the heart and looking at the shape and motion of the heart valves. This test may also be used to look for fluid around the heart and blood clots or masses inside of the heart or aorta.A blood pressure cuff will be placed on your arm. Small sticky patches, called electrodes, will be placed on your chest. An oxygen transducer will be placed on your finger to measure the amount of oxygen in your body. Your heart rhythm, blood pressure, oxygen levels, and breathing will be monitored during the test. You will be given oxygen.
An intravenous line (or IV) will be placed into a vein in your arm. A local anesthetic will be sprayed to numb the back of your throat. Medicine will be given through your IV to help you relax and feel sleepy. The doctor will gently insert the probe into your mouth. As you swallow, the probe will be directed into your esophagus. You may feel the probe moving, but it is generally not painful. When the probe is positioned in the esophagus just behind the heart, pictures of the heart will be taken. The test will take about 1 1/2 hours.
Treadmill stress testing is indicated for the diagnosis and prognosis of coronary artery disease (CAD). This is the initial investigation of choice in patients with a normal or near-normal resting ECG capable of performing adequate exercise.

Indications for treadmill testing include:
Venous ablation is a treatment procedure to help regulate blood flow by heating or freezing certain veins. Venous ablation procedures are performed when other treatments, such as medication and exercise, don’t work to improve the condition of varicose veins. This procedure only treats the symptoms of varicose veins rather than curing them.
Venous ultrasound (VUS) is a valuable tool for the assessment of lower limb venous disease. It can be used to both diagnose and guide treatment. Venous U/S has been valuable in assessing patients with chronic venous insufficiency (CVI) where clinical examination alone has led to conflicting results, especially in cases of superficial thrombophlebitis or isolated calf vein reflux.

Venous U/S enables the identification of incompetent valves, deep venous reflux and venous ectasia. Venography remains the gold standard method for evaluating the more proximal veins of the lower limb, but Venous U/S can be used as an alternative in selected cases, particularly when there are contraindications to venographic techniques.Venous U/S has been widely reported in the literature and has emerged as a valuable non-invasive tool for use in patients with venous disease. Venous ultrasound (VUS) is a valuable tool for assessing lower limb venous disease. VUS can be used both to diagnose and guide treatment of Venous Disease Venography remains the gold standard test, but Venous U/S can be used as an alternative when there are contraindications to Venography . Venous U/S has been widely reported and can serve as a non-invasive method for diagnosing lower limb veins. Venous U/S is a valuable tool for assessing the lower limb venous disease, and Venous U/S can be used to both diagnose and guide treatment. Venography remains the gold standard test for evaluating more proximal veins of the lower limb, but Venous U/S can be used as an alternative in selected cases when there are contraindications to Venography.
An Adenosine Myocardial Perfusion Imaging test uses a radioactive imaging agent (not a dye) to produce pictures of the heart muscle. The imaging agent gives off a small amount of radiation which can be seen with a special camera. The amount of radiation exposure during this test is very small and poses no health risk.

The test will help your doctor determine if there are areas of your heart that do not receive enough blood supply due to coronary artery disease. Areas of your heart that may have been damaged from a previous heart attack may also be seen.
Prior to the test, an IV will be started. During the rest portion of the test, you will receive an injection of the radioactive imaging agent, and pictures will be taken of your heart. For the stress portion of the test, a medication (Adenosine) will be given through the IV to simulate exercise by dilating the blood vessels of the heart. During the infusion, you will be continuously monitored for blood pressure, heart rate, rhythm, and ECG changes.
Carotid ultrasonography (carotid U/S) is an ultrasound of the carotid arteries. Carotids are the arteries in your neck that supply blood to your brain. A small transducer, similar to the one used for listening with a stethoscope, is placed on the patient’s neck next to their windpipe (trachea).


A Cardiac Catheterization allows a physician to examine a patient’s heart for pumping function, check for blockage in the arteries bringing blood to the heart, and measure pressures within the heart. Patients are usually given a mild sedative prior to the procedure. This will help you feel more relaxed and maybe a bit sleepy.This test is done in a room with special cameras to take x-ray pictures of your heart.
The nurse or technician will cleanse and shave the area and cover you with sterile drapes. The doctor will then numb the area and insert a small hollow tube or sheath into the artery in your groin (or arm). The physician can then thread special catheters (long, thin plastic tubes) up to the heart.This test is done in a room with special cameras to take x-ray pictures of your heart. Most cardiac catheterizations are done through a large artery in the groin, However Dr. De is known for being one of the few who prefer the radial approach, done through the wrist.
Through these specially shaped catheters, the physician can inject x-ray contrast dye and take x-ray pictures of the arteries that supply blood to the heart muscle and the main pumping chamber of the heart. Some people may notice a mild discomfort or “hot flash” following the dye injection which will last only a few seconds.
During the catheterization, the physician can view the x-ray images on special TV screens. The entire procedure can take as little as 20 minutes or sometimes more than an hour, depending on how many and what type of measurements are taken. After the physician has completed the procedure, the sheaths are removed from the groin (or arm) and a nurse or cath lab technician will hold pressure on the site to allow the small hole in the artery to close. A special dressing, pressure device or sandbag may be placed on the site at this time.
You will be asked to lie flat and still for several hours after the procedure to allow the hole in the artery to seal. Some physicians use a type of vascular closure device to seal the puncture in the artery. You should follow your physician’s specific instructions about activity following the use of one of these devices.
Most patients will go home several hours after the procedure, but because you have been given medication to relax you, please plan to have someone drive you home.

People who have had unexplained fainting spells or heart palpitations that can’t be detected by short term heart rhythm recording devices—such as Holter monitors—may be candidates for this device. Doctors may also recommend an implantable loop recorder for people with atrial fibrillation, which causes a rapid and irregular heartbeat. In addition, this device is used in people who have had a stroke for which a cause has not been determined.
Your doctor makes a small incision in the upper chest and inserts the device just under the skin. This is a brief, outpatient procedure done in our office, you can return to your usual activities the next day. Your doctor may limit your activity until the incision heals.
Cardiac loop recorders typically monitor the heart’s electrical activity for up to 36 months before replacement is required. The device is removed through the original incision site through a short surgery that is similar to the implantation procedure.

What is Peripheral Vascular Intervention?
Peripheral vascular intervention is a minimally invasive outpatient (same day) procedure used to treat peripheral artery disease, which causes plaque buildup in the arteries leading to the intestines, head, arms, and most commonly the legs. Plaque buildup is also called atherosclerosis.
The goal of peripheral vascular intervention is to restore the flow of blood to your lower extremities, eliminating pain, numbness, or need for amputation. Our specialists typically employ two different methods – angioplasty and atherectomy.
Angioplasty & Stents
Angioplasty is a minimally invasive intervention method that uses a balloon-tipped catheter to dilate your artery. Once inserted, the balloon is inflated at the blockage site to compress the plaque against the wall of the artery, increasing the flow of blood. In order to prevent the artery from becoming blocked again long-term, a small tube called a stent is sometimes put in place.
Atherectomy
Atherectomy is a non-surgical intervention that removes plaque using a catheter with either a sharp blade or a small drill on its tip. The plaque is either captured by the end of a catheter or is broken up and safely released into the bloodstream.


The sound waves reflect (echo) off the tissues and organs to create pictures which can be seen on a screen. The TEE provides very clear pictures of the heart structures and blood flow. The pictures are usually clearer than those obtained from a standard echocardiogram, which is performed from the chest wall. This test is often used to view hard-to-see structures or to obtain more detailed pictures of the heart and aorta.
Common reasons for the test include measuring the size and pumping strength of the heart and looking at the shape and motion of the heart valves. This test may also be used to look for fluid around the heart and blood clots or masses inside of the heart or aorta.A blood pressure cuff will be placed on your arm. Small sticky patches, called electrodes, will be placed on your chest. An oxygen transducer will be placed on your finger to measure the amount of oxygen in your body. Your heart rhythm, blood pressure, oxygen levels, and breathing will be monitored during the test. You will be given oxygen.
An intravenous line (or IV) will be placed into a vein in your arm. A local anesthetic will be sprayed to numb the back of your throat. Medicine will be given through your IV to help you relax and feel sleepy. The doctor will gently insert the probe into your mouth. As you swallow, the probe will be directed into your esophagus. You may feel the probe moving, but it is generally not painful. When the probe is positioned in the esophagus just behind the heart, pictures of the heart will be taken. The test will take about 1 1/2 hours.
Treadmill stress testing is indicated for the diagnosis and prognosis of coronary artery disease (CAD). This is the initial investigation of choice in patients with a normal or near-normal resting ECG capable of performing adequate exercise.

Indications for treadmill testing include:
Venous ultrasound (VUS) is a valuable tool for the assessment of lower limb venous disease. It can be used to both diagnose and guide treatment. Venous U/S has been valuable in assessing patients with chronic venous insufficiency (CVI) where clinical examination alone has led to conflicting results, especially in cases of superficial thrombophlebitis or isolated calf vein reflux.

Venous U/S enables the identification of incompetent valves, deep venous reflux and venous ectasia. Venography remains the gold standard method for evaluating the more proximal veins of the lower limb, but Venous U/S can be used as an alternative in selected cases, particularly when there are contraindications to venographic techniques.Venous U/S has been widely reported in the literature and has emerged as a valuable non-invasive tool for use in patients with venous disease. Venous ultrasound (VUS) is a valuable tool for assessing lower limb venous disease. VUS can be used both to diagnose and guide treatment of Venous Disease Venography remains the gold standard test, but Venous U/S can be used as an alternative when there are contraindications to Venography . Venous U/S has been widely reported and can serve as a non-invasive method for diagnosing lower limb veins. Venous U/S is a valuable tool for assessing the lower limb venous disease, and Venous U/S can be used to both diagnose and guide treatment. Venography remains the gold standard test for evaluating more proximal veins of the lower limb, but Venous U/S can be used as an alternative in selected cases when there are contraindications to Venography.
Venous ablation is a treatment procedure to help regulate blood flow by heating or freezing certain veins. Venous ablation procedures are performed when other treatments, such as medication and exercise, don’t work to improve the condition of varicose veins. This procedure only treats the symptoms of varicose veins rather than curing them.